Understanding Chemo Brain Fog: The Gut Connection Explained
Written on
Chapter 1: Introduction to Chemo Brain
Recently, I encountered a wonderful young woman who had just finished her chemotherapy for breast cancer. She expressed her frustration with treatment-related cognitive challenges, commonly referred to as "chemo brain," which includes memory and thinking difficulties. As a radiation oncologist, I frequently hear cancer survivors use this term to articulate the cognitive struggles they face during and after treatment. Similar complaints can arise from radiation therapy or hormonal treatments that inhibit estrogen. Despite the common usage of "chemo brain," the precise origins of these cognitive issues remain somewhat unclear.

Chapter 2: The Gut Microbiome's Role
Recent studies suggest a possible link between chemotherapy-induced brain fog and the gut microbiome. Let's take a closer look at the symptoms associated with chemo brain, the risk factors involved, and the emerging evidence pointing toward the gut's influence. Finally, I will provide some strategies for optimizing your microbiome.
Section 2.1: Symptoms of Chemo Brain
The symptoms of chemo brain are varied and often subtle, impacting different facets of cognitive performance. Individuals may find themselves feeling disorganized, confused, and struggling to focus. They might face challenges in retrieving the right words, learning new tasks, or multitasking efficiently. Many describe a constant feeling of mental haze, along with a diminished attention span and short-term memory issues. Routine tasks may take longer to complete, and difficulties with verbal and visual memory can complicate everyday life.
Section 2.2: Research Insights
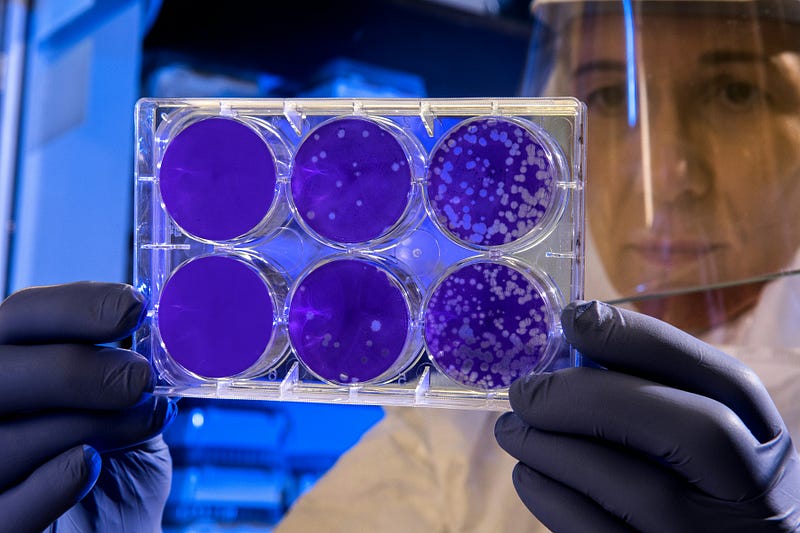
Researchers have explored the potential connection between the gut microbiome and cognitive functioning. In a longitudinal study, 77 women with breast cancer were monitored over time. Researchers collected fecal samples to analyze their gut microbiome, along with blood samples and cognitive assessments before, during, and after chemotherapy. This approach enabled an examination of changes in the gut microbiome and cognitive function throughout the treatment process.
Subsection 2.2.1: Study Methodology
The study involved visiting women with breast cancer at three significant points during their treatment. The initial visit took place before chemotherapy began, where baseline measurements of their gut microbiome were obtained through fecal samples. Blood samples were also taken to assess inflammatory immune markers, and cognitive tests were administered to establish initial cognitive function.

Section 2.3: Findings and Implications
During the second visit, which coincided with the last chemotherapy infusion, researchers repeated the collection of fecal and blood samples and reassessed cognitive function. The final visit occurred about three months after chemotherapy, allowing for a comprehensive evaluation of the long-term effects of treatment on both the gut microbiome and cognitive abilities.
The study revealed significant findings: alterations in the gut microbiome's community structure due to chemotherapy and elevated levels of circulating tumor necrosis factor-alpha. While participants reported cognitive decline, there was no direct correlation between these self-reported symptoms and changes in the gut microbiome or inflammatory markers.

However, a noteworthy observation emerged: declines in objective cognitive performance were linked to reduced microbial diversity, independent of circulating inflammatory cytokines. This suggests that the diversity of the gut microbiome may play a crucial role in cognitive health.
Section 2.4: Exploring Alternative Mechanisms
Further analysis indicated distinct taxonomic changes within the gut microbiome of patients experiencing cognitive decline, compared to those who did not. These specific bacterial patterns could provide insights into the microbes involved in cognitive impairment following chemotherapy. Interestingly, the study found that cognitive decline was associated with changes in the gut microbiome rather than inflammation. This challenges the traditional view that immune system activation is the primary communication pathway in chemo brain.

The authors propose that metabolites produced by the gut microbiome, such as short-chain fatty acids and bile acids, might significantly influence brain function. Disruptions in the gut microbiome could alter the levels and composition of these metabolites, potentially leading to cognitive decline.
Chapter 3: Practical Implications for Health
What can we take away from this study? There are practical implications for our health, particularly concerning the microbiome's role. A healthy microbiome is linked to overall health, including:
- Gut health
- Heart health
- Weight management
- Blood sugar regulation
Section 3.1: Tips for Enhancing Your Gut Microbiome
To support a healthy gut microbiome and potentially reduce the risk of chemo brain, consider the following dietary and lifestyle changes:
- Embrace Dietary Diversity: Incorporate a wide range of foods, especially legumes, beans, and fruits, which are high in fiber and beneficial for promoting Bifidobacteria.
- Ferment for Gut Health: Add fermented foods like yogurt, sauerkraut, and kefir to your diet to introduce healthy bacteria, particularly Lactobacilli.
- Limit Artificial Sweeteners: Reduce or eliminate artificial sweeteners like aspartame, as they may foster unhealthy bacteria and disrupt blood sugar levels.
- Prioritize Prebiotic Foods: Include foods such as artichokes, bananas, asparagus, oats, and apples, which nourish beneficial gut bacteria.
- Breastfeed for Optimal Gut Development: For infants, breastfeeding for at least six months is crucial for developing a healthy gut microbiome.
- Choose Whole Grains: Opt for whole grains instead of refined ones, as they are rich in fiber and beneficial carbohydrates that support gut health.
- Explore Plant-Based Options: Consider integrating more plant-based meals into your diet to reduce harmful bacteria and inflammation.
- Indulge in Polyphenol-Rich Foods: Enjoy foods like red wine, green tea, dark chocolate, olive oil, and whole grains, which can stimulate the growth of beneficial bacteria.
- Consider Probiotic Supplements: Probiotics can help restore a healthy gut microbiome after disruptions by repopulating it with beneficial microbes.
- Use Antibiotics Judiciously: Use antibiotics only when necessary, as they can upset the delicate balance of the gut microbiome.
In summary, consuming a varied diet rich in fiber and fermented foods is vital for maintaining a healthy microbiome and may help mitigate the risk of cognitive issues associated with chemotherapy.
Chapter 4: Conclusion
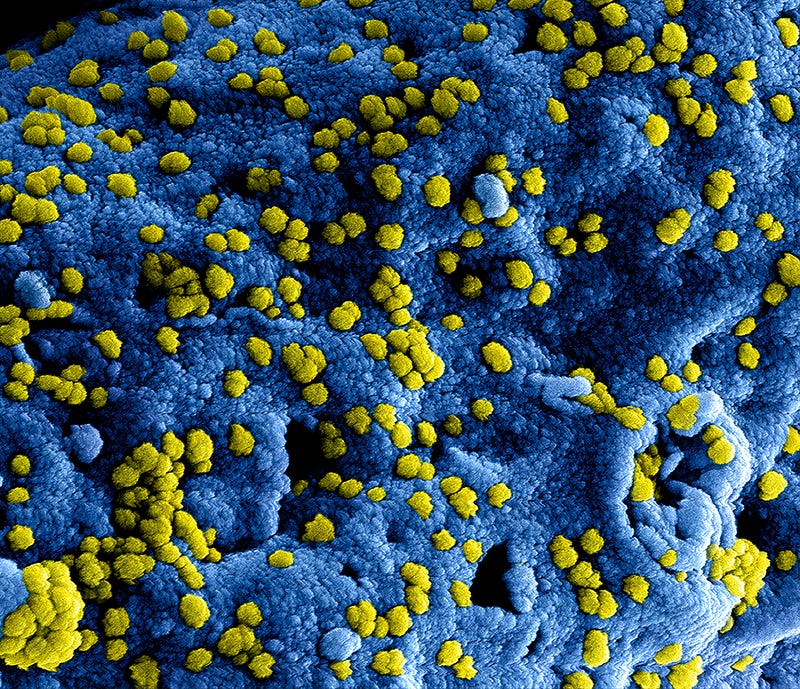
The gut microbiome consists of trillions of microorganisms that influence various aspects of health, including brain function. Understanding how our gut health affects cognitive performance can be a crucial step toward improving overall well-being.
Thank you for exploring "Understanding Chemo Brain Fog: The Gut Connection Explained."