Understanding Sudden Cardiac Death: Prevention and Treatment
Written on
Chapter 1: Overview of Sudden Cardiac Death
Sudden cardiac death (SCD) refers to an unexpected death that occurs in an individual who appears healthy or one who may have a chronic condition but is in a stable or improving state. We define "sudden" as death occurring within one hour following the onset of alarming symptoms.
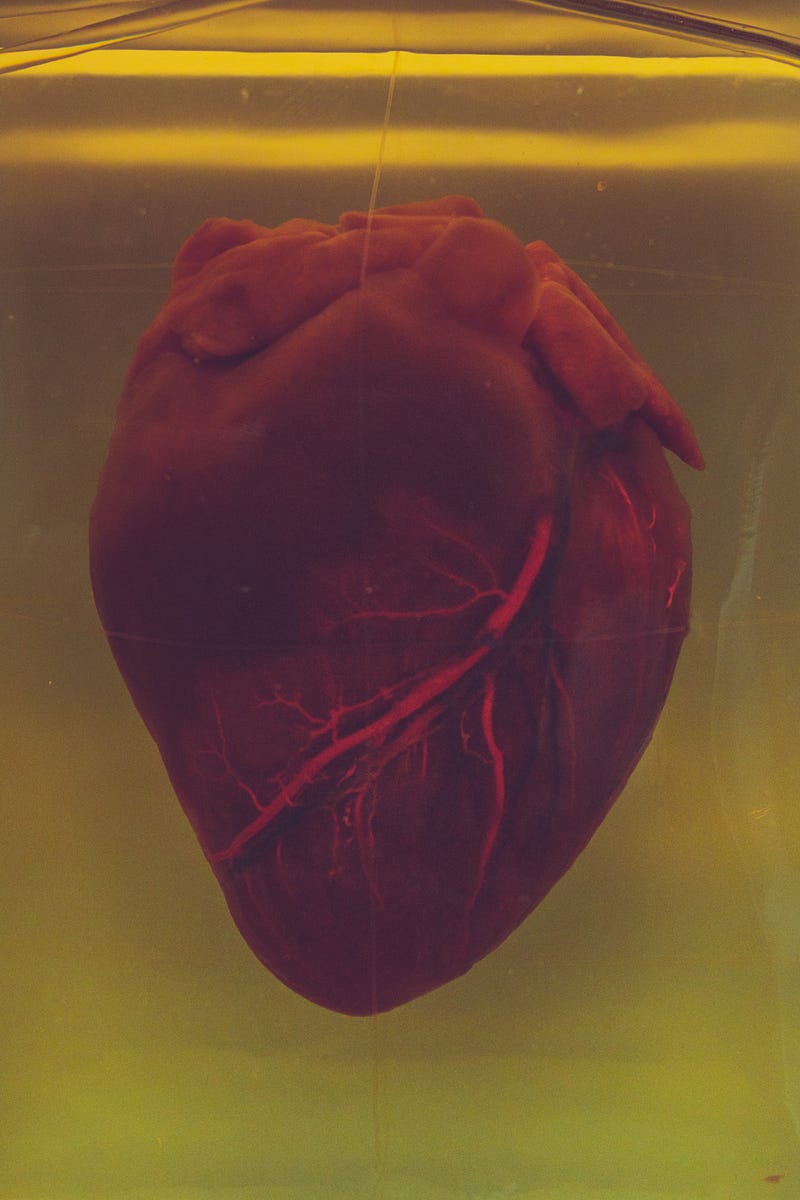
Photo by Camilo Jimenez on Unsplash.
This phenomenon poses a significant challenge in modern medicine. According to the U.S. Mortality Survey, between 400,000 to 460,000 individuals in the United States succumb to sudden cardiac death annually, either in emergency departments or before reaching a hospital. Typically, patients may experience intense chest pain, palpitations, fainting spells, extreme fatigue, profuse sweating, shortness of breath, and dizziness before the event.
Section 1.1: What Is Sleep Apnea?
Sleep apnea is a prevalent condition that is thought to affect approximately 22 million individuals in the United States.
Chapter 2: Causes of Sudden Cardiac Death
Sudden cardiac death can result from several factors, including:
- Acute mechanical heart failure, often linked to myocardial infarction, which can cause the heart wall to rupture.
- Severe arrhythmias that directly impact the patient's hemodynamic stability. The arrhythmias that lead to SCD are not the benign irregularities experienced during stress; rather, they are serious conditions that can cause immediate hemodynamic collapse, preventing the heart from effectively pumping blood to the body. The main culprits are ventricular tachycardia and ventricular fibrillation.
The only chance for recovery lies in swift medical intervention and defibrillation using an external defibrillator, which helps restore normal heart rhythm. These devices are commonly found in hospitals, health centers, and busy public areas like airports, and their operation requires specialized training.
Redefining Sudden Cardiac Death with the POST SCD Study - YouTube
This video explores the latest research and insights into sudden cardiac death, shedding light on preventive measures and treatment options.
Section 2.1: Prevention Strategies
Unfortunately, immediate responses may not always be feasible, leading to the necessity for effective prevention strategies against sudden arrhythmic cardiac death. Early diagnosis and treatment of underlying heart conditions are vital to prevent fatal outcomes. All possible actions should be taken to manage heart disease before it culminates in sudden death. If prevention isn’t viable, a crucial tool in our medical arsenal is the implantable defibrillator.
What is SCD (sudden cardiac death) - YouTube
This informative video provides an overview of sudden cardiac death, its causes, risk factors, and what can be done to mitigate these risks.
Section 2.2: Conditions Associated with Increased Risk
Certain diseases elevate the risk of developing severe arrhythmias, including:
- Coronary heart disease, especially with a history of myocardial infarction.
- Dilated cardiomyopathy.
- Hypertrophic cardiomyopathy.
- Valve diseases.
- Genetic disorders like Long QT Syndrome, Brugada Syndrome, and others.
The notable decrease in sudden arrhythmic cardiac death rates observed in extensive multicenter studies utilizing implantable defibrillators has led to a rise in annual implants and broader indications for their use.
Chapter 3: The Role of Implantable Defibrillators
An implantable defibrillator is a sophisticated electrical device, akin to external defibrillators used in hospitals. It functions as a pacemaker, providing assistance in cases of bradycardia and fatal arrhythmias. It detects irregular heart rhythms, activates automatically, and administers energy to correct the dangerous arrhythmia, allowing patients to avoid immediate hospitalization while still receiving 24/7 protection against life-threatening arrhythmias. This advancement represents a significant leap in medical technology.
Section 3.1: Patient Selection for Implantation
Initial studies indicate that these devices should be placed as secondary prevention for patients who have survived a sudden arrhythmic event with medical assistance. However, they may also be implanted in high-risk patients as a primary preventive measure.
Section 3.2: Installation Process
These devices are implanted similarly to pacemakers, under local anesthesia in a hospital setting. The procedure involves placing electrodes and a generator. The electrodes are threaded through a large vein into the heart chambers, while the generator is positioned subcutaneously beneath the skin. A specialized cardiologist programs the device externally to monitor heart rhythms continuously and respond to abnormalities.
Section 3.3: Lifestyle Considerations
Patients with an implantable defibrillator need to avoid high magnetic fields, which are rare in everyday life. It is advisable to use mobile phones on the opposite side of the implant.
Section 3.4: Effectiveness of Implantable Defibrillators
These devices have proven highly effective, reducing overall mortality by 35–40% in high-risk patients. Considering they are sometimes placed in young, healthy individuals with genetic conditions, it is clear they play a vital role in enhancing survival rates among those at risk of sudden arrhythmic death.